Scientists have discovered that hyperactive brain cells are responsible for elevated blood sugar in diabetes, challenging conventional understanding of the disease and potentially opening new treatment pathways. The finding, published May 15 in the Journal of Clinical Investigation, reveals that a specific set of neurons in the hypothalamus plays a crucial role in diabetes development that’s separate from their influence on body weight or food intake.
In a study using diabetic mice, researchers at the University of Washington found that silencing hyperactive AgRP neurons in the brain normalized blood sugar levels for months without affecting weight or eating habits. This discovery suggests that diabetes treatments targeting these neurons might help patients manage blood sugar even without weight loss.
“These neurons are playing an outsized role in hyperglycemia and type 2 diabetes,” said UW Medicine endocrinologist Dr. Michael Schwartz, corresponding author of the paper. He noted that the finding is a “departure from the conventional wisdom of what causes diabetes.”
Challenging Traditional Views
Type 2 diabetes has traditionally been understood as a peripheral disease caused by insulin resistance in tissues like muscle and liver, often tied to obesity and lifestyle factors. The brain’s role in diabetes development has received far less attention.
But growing evidence has prompted scientists to reconsider this view. The researchers had previously shown that injecting a protein called fibroblast growth factor 1 (FGF1) directly into the brain could normalize blood sugar in diabetic mice for extended periods.
Could hyperactive AgRP neurons be the key? To find out, the team used a genetic technique to silence these neurons in obese, diabetic mice.
The results were striking: blood sugar levels fell from diabetic range (above 200 mg/dL) to normal range (around 140 mg/dL) within a week and remained stable for the entire 10-week study period. Yet food intake, body weight, fat mass, and energy expenditure remained unchanged.
The Brain-Diabetes Connection
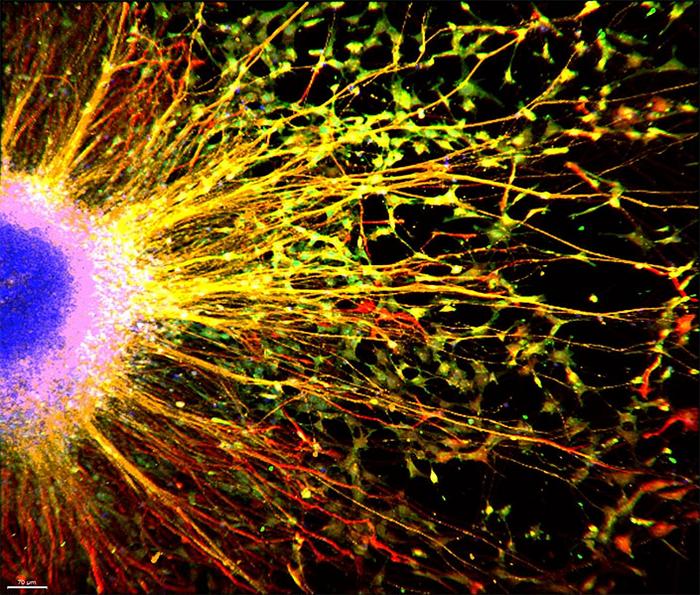
To permanently inactivate AgRP neurons, researchers injected a virus carrying tetanus toxin into the arcuate nucleus of the hypothalamus where these neurons reside. The toxin prevents neurons from communicating with other cells but doesn’t kill them.
When examining the physiological changes accompanying normalized blood sugar, the team found several intriguing patterns:
- Plasma insulin levels dropped significantly, suggesting improved insulin sensitivity
- Liver glycogen content increased, indicating better liver glucose processing
- Plasma corticosterone (the mouse equivalent of cortisol) levels decreased
- Plasma lactate levels increased, possibly supporting enhanced hepatic glucose uptake
Interestingly, the researchers found no changes in liver fat content or gluconeogenic gene expression, suggesting the improvement in blood sugar control works through different mechanisms than traditional diabetes treatments.
Separating Obesity from Diabetes
Perhaps the most surprising aspect of the study was how silencing AgRP neurons normalized blood sugar without affecting body weight or food intake. This challenges the assumption that obesity and diabetes are inseparably linked.
“While these neurons are important for controlling blood sugar in diabetes, they don’t play a major role in causing obesity in these mice,” the researchers noted in their report.
What makes this finding particularly interesting is that it suggests different brain circuits might separately control metabolism and eating behavior. This could explain why some diabetes treatments work effectively even without significant weight loss, while others require weight reduction to improve blood sugar control.
Implications for Human Treatment
Could these findings translate to humans? While mouse studies don’t always predict human outcomes, there are intriguing connections to current diabetes treatments.
Schwartz noted that popular GLP-1 receptor agonist medications like Ozempic are known to inhibit AgRP neurons. “The extent to which this effect contributes to the antidiabetic action of these drugs is unknown,” he said, suggesting a potential mechanism for how these medications work beyond weight loss.
The research also aligns with growing evidence that the brain plays a significant role in metabolic regulation. Multiple studies have shown that interventions targeting the central nervous system can profoundly affect glucose metabolism throughout the body.
Looking Ahead
More research is needed to understand how these neurons become hyperactive in the first place and how to safely regulate their activity in humans. But the findings suggest new possibilities for targeted diabetes therapies that might work independently of weight loss.
How might such treatments work? They could potentially involve medications specifically designed to dampen AgRP neuron activity or leverage existing drugs that affect these neurons as part of their mechanism.
As researchers continue to unravel the brain’s role in diabetes, these findings challenge us to think differently about this common disease. Rather than viewing type 2 diabetes solely as a peripheral metabolic disorder driven by obesity, we may need to consider it partly as a disorder of brain function – one where hyperactive neurons drive high blood sugar independently of body weight.
This perspective shift could ultimately lead to more effective treatments for a disease that affects hundreds of millions of people worldwide.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!