Summary: A new study suggests that gabapentin, a widely used anti-seizure medication, may improve survival in patients with glioblastoma (GBM), the deadliest form of brain cancer. Researchers found that GBM patients taking gabapentin lived several months longer than those who did not, across two independent hospital datasets.
The findings stem from insights into how brain tumors exploit neural signaling, with gabapentin potentially disrupting this interaction by lowering levels of a key protein, thrombospondin-1 (TSP-1). While promising, the study is retrospective and calls for randomized trials to validate gabapentin as a therapeutic option for GBM.
Key Facts:
- Survival Benefit: GBM patients on gabapentin survived 4–6 months longer on average.
- Biological Marker: Gabapentin use was linked to lower serum TSP-1, a tumor-promoting protein.
- Broad Dataset: Findings were replicated in over 1,000 patients across two medical centers.
Source: Mass General
A new study by investigators from Mass General Brigham suggests that gabapentin, a relatively common anti-seizure/pain medication, is linked to improved survival in patients with glioblastoma (GBM) — the most common and deadly form of brain cancer in adults.
The findings, published in Nature Communications, are based on a retrospective analysis and add new evidence to help patients with this devastating disease.

“This study is an exciting step forward,” said lead author Joshua Bernstock, MD, PhD, a clinical fellow in the Department of Neurosurgery at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system.
“GBM is a relentlessly progressive and nearly universally fatal disease.
“The discovery that an already approved medication with a favorable safety profile can extend overall survival represents a meaningful and potentially practice-changing advance.”
GBM is a highly aggressive and deadly form of brain cancer. With about 12,000 new cases diagnosed annually in the United States, GBM accounts for most primary brain tumors in adults.
Overall survival has barely improved over the last several decades, with most patients living only 12 to 14 months after diagnosis and 5.5 months after recurrence.
The new study was sparked by insight from the field of cancer neuroscience. This research area focuses on how tumors manipulate neural signaling to fuel their growth.
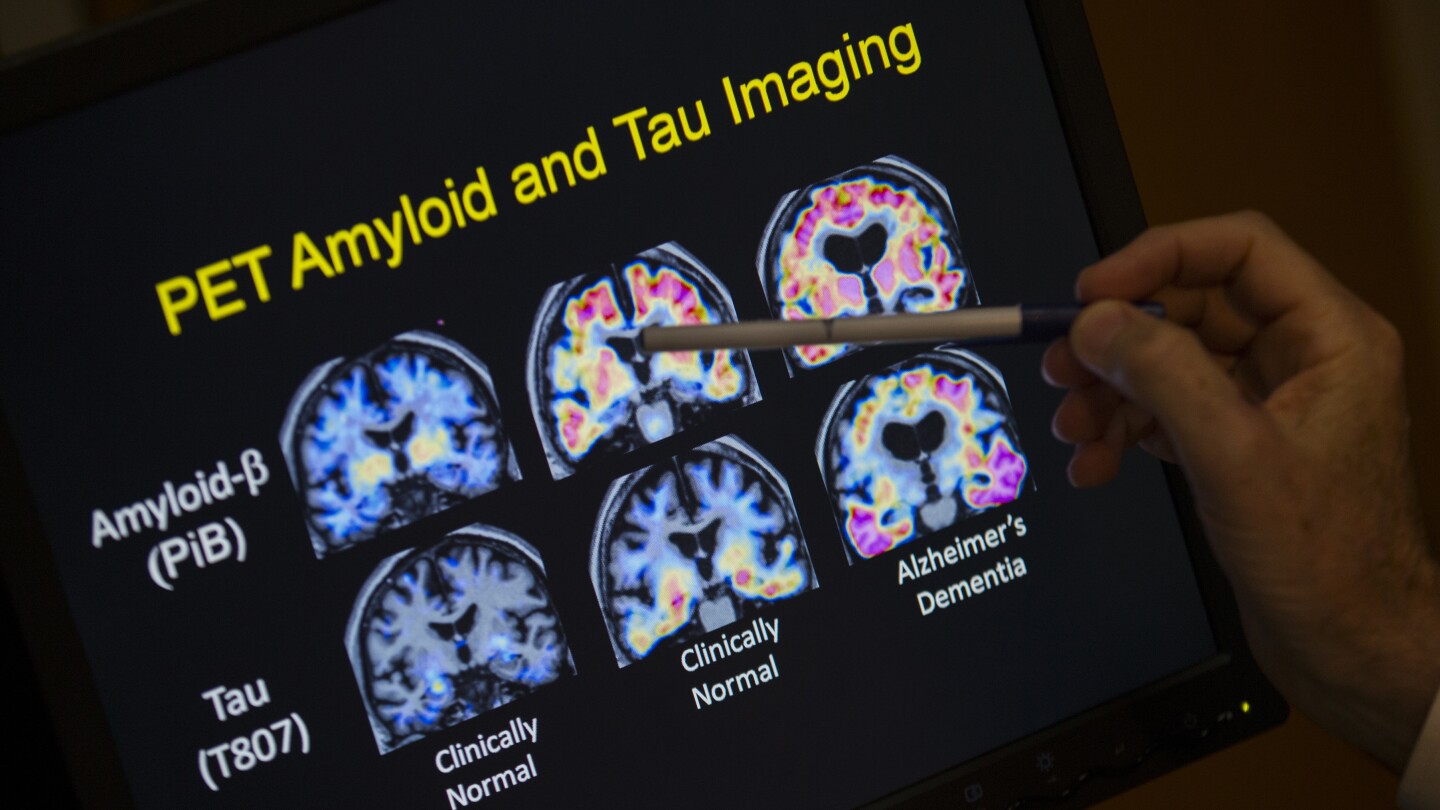
A 2023 study published in Nature identified thrombospondin-1 (TSP-1)—a protein involved in neural circuit development and remodeling—as a key mediator of interactions between neurons and tumor cells that promote glioma growth.
In mouse models, this neuron–tumor axis was successfully targeted using gabapentin, suggesting a potential therapeutic strategy.
Intrigued by this research, Bernstock and colleagues analyzed the outcomes of 693 GBM patients at Mass General Brigham. Many of the patients were already taking gabapentin for reasons that typically centered on nerve pain.
Those who were taking the drug survived an average of 16 months compared to 12 months for those who weren’t. This four-month survival benefit was statistically significant.
Because the results seemed “almost too good to be true,” according to Bernstock, he connected with Dr. Shawn Hervey-Jumper’s team at University of California, San Francisco (UCSF) to add to the dataset and discovered they were able to replicate what was found at Mass General Brigham.
Of the 379 patients with newly diagnosed GBM included in the UCSF cohort, patients on gabapentin survived an average of 20.8 months, while those not taking gabapentin survived an average of 14.7 months. Together, the data included 1,072 patients and found a significant survival benefit.
The study also found that patients treated with gabapentin had lower levels of serum TSP-1, suggesting that the protein may serve as an indicator of treatment response. However, the relationship between TSP-1 levels and gabapentin needs further investigation, Bernstock said.
“There have been very few advances in survival for GBM patients since the early 2000s,” Bernstock said. “We need to think more creatively about the emerging biology in these tumors and how to target them.”
While the findings are promising, the study is retrospective — the researchers didn’t give patients gabapentin in a controlled way to test its effects. Bernstock stressed that larger, randomized clinical trials are needed to confirm the results and explore the role of gabapentin and TSP-1 in GBM progression.
About this brain cancer and neuropharmacology research news
Author: Liz Murphy
Source: Mass General
Contact: Liz Murphy – Mass General
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Gabapentinoids confer survival benefit in human glioblastoma” by Joshua Bernstock et al. Nature Communications
Abstract
Gabapentinoids confer survival benefit in human glioblastoma
Neuronal-glioma interactions are increasingly recognized as critical in the development and progression of central nervous system tumors.
Recent research highlights that gliomas can integrate into neural circuits through various mechanisms, including the synaptogenic factor thrombospondin-1 (TSP-1).
This new mechanistic understanding of cancer neuroscience allows for novel insights into target discovery.
Critically, therapies that modulate neuron-tumor interactions remain agnostic to other oncogenic changes within tumor cells yet may still target fundamental drivers of tumor growth.
In line with these findings and controlling for critical confounding variables, we demonstrate a survival benefit associated with gabapentin (an antagonist of TSP-1) following surgical resection of newly diagnosed glioblastoma.
This retrospective, multi-institutional cohort study included 1,072 patients, with a discovery cohort of 693 patients and an additional 379 patients from a separate site for external validation.
Furthermore, our findings indicate that gabapentin administration is associated with reduced serum TSP-1 levels, suggesting its potential as a future biomarker.